Being Pro-Life: Palliative Care: It’s Not Just for End of Life
 Jill’s mother was living a full life with Parkinson’s disease for 20 years, until she recently developed much worse symptoms, including dementia. She began seeing a memory care specialist and was prescribed medication, but that seemed to make her dementia worse. She also started showing signs of serious gastrointestinal distress, which could be a symptom of Parkinson’s or her medication. After months of consultation with differing specialists, she went to the emergency room where doctors discovered that she had an obstructed bowel, a serious complication from a previous hernia mesh surgery.
Jill’s mother was living a full life with Parkinson’s disease for 20 years, until she recently developed much worse symptoms, including dementia. She began seeing a memory care specialist and was prescribed medication, but that seemed to make her dementia worse. She also started showing signs of serious gastrointestinal distress, which could be a symptom of Parkinson’s or her medication. After months of consultation with differing specialists, she went to the emergency room where doctors discovered that she had an obstructed bowel, a serious complication from a previous hernia mesh surgery.
During her recovery, she was kept on heavy pain medication much longer than her family thought necessary. While recovering at home, she fell and broke her arm. It was not a serious break, so she was given a soft, removable cast, despite the family’s concerns that her dementia would likely make her want to remove it. As predicted, she removed the cast and re-injured her arm to the point of needing surgery.
Believe it or not, this is the perfect scenario for palliative care. Most people associate palliative care with hospice care or pain management for dying people. While palliative care is appropriate for that situation, it is much broader than just that. Palliative care focuses on relieving the symptoms and stress of any serious medical condition, at any age and any stage, even while pursuing curative treatment. It involves doctors, nurses, social workers and even chaplains.
While a medical specialist typically focuses on the immediate needs of an illness/injury, its effects are much broader. Palliative care helps deal with many other questions like: How does this course of treatment relate to my other medical conditions? How can I anticipate what this will mean for my life long term? How do I make decisions in line with what my Catholic faith teaches?
All of these questions should inform decisions on treatment, but without a palliative care specialist involved, a family is often left alone with these questions. All too often, they feel unsupported by medical professionals.
Other than the end of life, when might someone need palliative care? Dr. Tim Jessick, a palliative care specialist, mentioned three common situations:
1. You are dealing with two or more specialists at one time.
2. A patient is frequently being admitted to the hospital (several times in a few months).
3. There is a big decision to be made about aggressive care.
Ask for It
Most hospitals today have an interdisciplinary team for palliative care, but most medical specialists do not realize when such referrals are appropriate, so families need to request it. Denise Hess, executive director of the Supportive Care Coalition (a Catholic coalition which supports and advocates for palliative care), shared that a recent study showed 71 percent of the U.S. population had never heard of palliative care, much less understood what it is.
Get Involved
First, educate yourself so that you and your loved ones know to ask for palliative care when the need arises. Go to our website for links to stories on how palliative care was helpful to people in various situations. Use these resources to host an education night at your parish.
Additionally, there is a bill currently in the U.S. Senate called the Palliative Care and Hospice Education and Training Act that is supported by the United States Conference of Catholic Bishops. Contact your senators and ask them to support this bill to improve the availability of palliative care across the country.
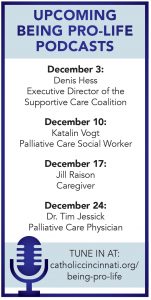
Watch the interviews online and subscribe to the podcast at www.catholiccincinnati.org/being-pro-life.
 Bob Wurzelbacher is the director of the Office for Respect Life Ministries. He and his wife, Cindy, live in Sharonville with their two young daughters.
Bob Wurzelbacher is the director of the Office for Respect Life Ministries. He and his wife, Cindy, live in Sharonville with their two young daughters.
[email protected]