Hospice care helps patients, families find peace as death nears
Thursday, October 28, 2010
By Eileen Connelly, OSU
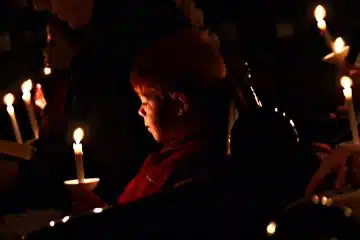
ARCHDIOCESE — There is no easy way to lose a loved one, but hospice programs can make the end-of-life journey a more sacred and peaceful one for patients and their families.
Hospice provides physical, emotional and spiritual care for terminally ill patients and their families. It is available when a doctor has indicated a patient’s life expectancy is six months or less if the disease takes its normal course. The great majority of hospice patients incur no out-of-pocket costs for medical equipment, supplies and services related to the terminal illness because hospice services are covered by the Medicare hospice benefit as well as most private insurance plans.
Sandra Lobert, president/CEO of Hospice of Cincinnati, stresses that hospice is not a place, but a philosophy.
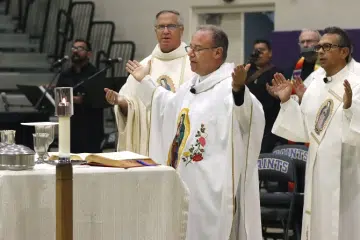
 |
| Raymond Guye and his wife, Mary, who passed away at Hospice of Cincinnati in August, posed with their seven grandchildren last Easter. (Courtesy photo) |
“Our focus is on comfort, rather than curative care. Our focus is on the patient,” she said. “Hospice is the model for quality, compassionate care for facing a life-threatening illness. We provide expert medical care, pain management and emotional and spiritual support expressly tailored to patient’s needs and those of their loved ones, in an atmosphere of sensitivity and respect.”
The hospice philosophy is supported by church teaching that only God can chose when to end a human life. Families can, however, if the patient is unable, choose to make a loved one’s passing as comfortable as possible, even if doing so may shorten his or her life.
The Catechism of the Catholic Church states, “Discontinuing medical procedures that are burdensome, dangerous, extraordinary or disproportionate to the expected outcome can be legitimate; it is the refusal of ‘overzealous treatment.’ Here one does not will to cause death; one’s inability to impede it is clearly accepted. The decisions should be made by the patient if he is competent and able or, if not, by those legally entitled to act for the patient, whose reasonable will and legitimate interests must always be respected” (Paragraph #2278).
Many patients could benefit from hospice care long before inquiring about it, say program directors. The option is often delayed because patients, family members or doctors don’t mention hospice out of concern that someone might be anxious or uncomfortable discussing death.
“Sometimes an initial barrier is that people see hospice as giving up,” Lobert said. “But recent studies (in The Journal of Pain Management) show that hospice care actually extends life. That’s the best way to think about it. You may be dying, and there’s clearly the expectation that you may die when entering our program, but we have people we discharge who do get better.”
Hospice care focusses on the individual goals of the patient and “the quality of time” they have left, she said. Rather than dealing with the effects of aggressive, curative treatment, patients are able to focus on “connecting with their families and whatever brings them the most joy. Our goal is to help the patients and their families through a trying, and some would say, very sacred time. There’s a difference in the quality of one’s death; you can have a good death or a bad death. Many people die without their family members present, connected to tubes. We want to offer patients peace, comfort and a little bit of joy.”
Raymond Guye, whose wife, Mary, passed away at Hospice of Cincinnati’s inpatient care center in Blue Ash on Aug. 9, said this was their experience. The mother of three and grandmother of seven was initially diagnosed with breast cancer 16 years ago. She was given the “all clear” after a mastectomy, her husband said, but in 2009 the couple learned the cancer had metastasized. Aggressive treatment followed, but in March her oncologist informed the husband and wife of 44 years that the cancer was terminal.
In his wife’s room at Bethesda North Hospital, the couple listened to the doctor explain options for ongoing care.
“We weren’t really concentrating on what they were saying,” Guye recalled. “We didn’t really know what it was all about. We just knew Mary wanted and needed comfort care.”
After the couple had digested the information, they realized how closely the hospice philosophy is related to their faith.
“We talked about how God has a plan for each us,” Guye said. “We don’t always know what it is or may not understand, but we signed on to trust Him. We said ‘Thy will be done.’”
“We all wanted to take one day at a time and not worry about the future. We didn’t want to think about the how or when,” he added. “Hospice really tuned into where we were and respected that.”
Because Mary Guye was expected to live at least another two to three months and was still enjoying a good quality of life, a plan for her care was established that included services and a team dedicated to her comfort while she remained at home. Her husband served as her primary caregiver, and a hospice case manager/nurse came to the house for regularly scheduled visits once a week.
“She was very, very reassuring and helped us get into a routine,” Guye said. “Mary and I would talk before she came, then ask [about] any questions we had. Her recommendations were always supportive, but couched in reality. She communicated regularly with the oncologist and if anything regarding Mary’s care needed to be changed or added, it happened seamlessly.”
His wife was initially able to still enjoy the activities that were important to her — attending Sunday Mass at St. Michael Parish in Sharonville, strolling around their yard as warm weather broke and spending time with family. The couple’s son and daughter-in-law and their five children live nearby and would come by in the evening as often as possible to pray the rosary with them, he said.
As her conditioned weakened, a hospice home health aide began visiting to help provide assistance with daily activities and enable Guye to run errands. By early August, his wife needed constant supervision and was becoming increasingly agitated. She was entering the final phase of her illness.
“They prepared me well,” Guye said. “I knew when it was time to make the call. It was the right decision at the right time, and I remember saying ‘Thank you, God.’ Mary and I had talked about it and made peace. We said our goodbyes as she was leaving here. She gave me a small, demure smile and wave from the transport vehicle.”
At the inpatient center, the hospice staff was able to calm their new patient. A chaplain was available for spiritual support, and because patients and families are also welcome to have their own clergy members visit, Jesuit Father Peter Carey, a family friend, arrived to anoint her.
The nurses, whom Guye refers to as “the A-Team,” “were very helpful and very reassuring. They never did a thing without first explaining why they were doing it. They really took comfort care into their hearts and souls. They are people with a spirit of faith, a spirit of hope.”
Since his wife’s death, Guye has participated in a grief support group at Good Shepherd Parish in Montgomery, which he finds helpful. Hospice of Cincinnati also offers a wide range of counseling services for friends and families of patients, including grief support groups, individual and family counseling, memorial services, special interest seminars and Fernside, a center for grieving children.
“I really believe people should take advantage of opportunities to help with their grief after a love one dies,” Lobert said, noting that Hospice of Cincinnati’s grief support services are open to the entire community.
Guye, who presides at Communion services at his parish, along with taking the Eucharist to the sick and shut-ins, is considering becoming a volunteer at Hospice of Cincinnati in the future, but will wait the required year following the loss of a loved to make any decisions.
Meanwhile, he is keeping active and trying to “decide what my calling down the road will be.”
Reflecting on his wife’s end-of-life journey, Guye said, “I wouldn’t change a thing. We had so much support from our family and from hospice, and so much faith in God. There were good days and there were better days, and every day Mary I had together, we felt blessed.”
CNS also contributed to this story.